In Search of the Water Pump: Architecture and Cholera
It had once been the manicured lawn of the sixth-hole fairway on the outer rim of Port-au-Prince. I could still make out the course’s manipulated topography, its rolling hills designed as obstacles to trap and deflect golf balls, its flattened greens to launch them, and a tree-less drive—all to capture feckless mastery over nature. But in 2010, after the earthquake in Haiti, there was very little ambiguity about which force was in control.
The Pétionville Club was now a city of mud. Open sewers overflowed with trash and human waste, and caked earth was layered between recently erected tents. Mothers clutching babies and feral dogs huddled around nameless masses wrapped in blankets bearing the barely insouciant byline “From the American People” stamped all over them. I had never imagined a city like this. But the Pétionville Club was now a city. It was a city because gangs gathered to control the water pumps. It was a city because plastic bottles piled high in cordoned garbage zones while tents swayed against each other into faint street corridors. It was a city because when cholera broke out a few months after its settlement, it erupted as it only could in a city—through waste, through water contaminated with that waste, and through the consumption of that wastewater by people living so close together that one could hardly hold on to the lingering illusion that we just might be independent beings. But unlike any city of the recent past, the Haitian cholera outbreak spread more rapidly and aggressively than any city had seen in over 100 years.
It sometimes takes a disaster to reveal the fraying threads that undergird the social fabric of a place. In December 2011, cholera was that tear, uncovering the true structural consequences of a country with so much broken building stock. The outbreak also revealed that it was not a lack of medical care or drugs or good intentions that paved Haiti’s road to hell, but the very real and alarmingly limited number of working wastewater pipes that lay beneath it. What enabled cholera and crippled Haiti was a complete failure of the built environment.
As with many outbreaks, the response was more slow than swift. Emergency tents popped up, doctors gloved up, and bilaterals pledged up. And yet, when the disease broke, the capital’s only waste-filtration plant remained closed, and privatized removal companies were caught illegally dumping waste back into the ground. Meanwhile, residents continued to do what had always been done—to defecate openly and to collect water from gutters on the side of the road. Nocturnal frogmen called the bayakou shoveled out overflowing latrines and in the dawn hours dumped them along roadside pits, leaving the sewage to seep deep into ground soil. Over time, the cholera cases began to wane, the tents were removed, and the nation emerged with one quarter of its populace lacking safe sanita- tion and a third without clean water—returning largely to its state before the outbreak.
Cholera
In spite of what the outbreak in Haiti suggests, cholera is a preventable and treatable disease. However, in the 19th century, it was the new plague—“the wasting death,” “the midnight raid”—that turned cities into ghost towns overnight and crossed the globe faster than any clipper ship could have dreamed. Steven Shapin’s 2006 New Yorker essay “Sick City” describes cholera as the pandemic disease whose breadth was fueled by the “‘great tracks of human intercourse’—colonialism and global trade.”1 The deaths were staggering. The first pandemic, which began in Calcutta in 1817, killed hundreds of thousands by the time it ended in 1824. The second pandemic came in 1826 and traveled to Great Britain where it killed some 20,000 people in less than two years. By 1854, another 80,000 people had died in two subsequent outbreaks. The world was besieged.
And few understood why. Cholera seemed to afflict the poorest residents most severely, and those living in overcrowded tenements were scourged by any number of social and public ills. Shapin quotes Charles E. Rosenberg’s The Cholera Years: “Medical opinion was unanimous in agreeing that the intemperate, the imprudent, the filthy were particularly vulnerable.”2 Epidemics like cholera, and later HIV/AIDS, have long been used to reinforce puritanical prejudice and the moral superiority of class. Haiti’s experience today is no different.
As moral theories fester, though, they also breed skepticism. And one young London doctor, John Snow, sought a scientific reason why a disease was running rampant through the newly minted capitals of industrial wealth.
In the 1840s, London’s Soho was a thick layer cake of tenements separated only by the narrow footpaths sliced like random incisions of unequal portions. A prime breeding ground, it turned out, for the 1854 cholera outbreak.
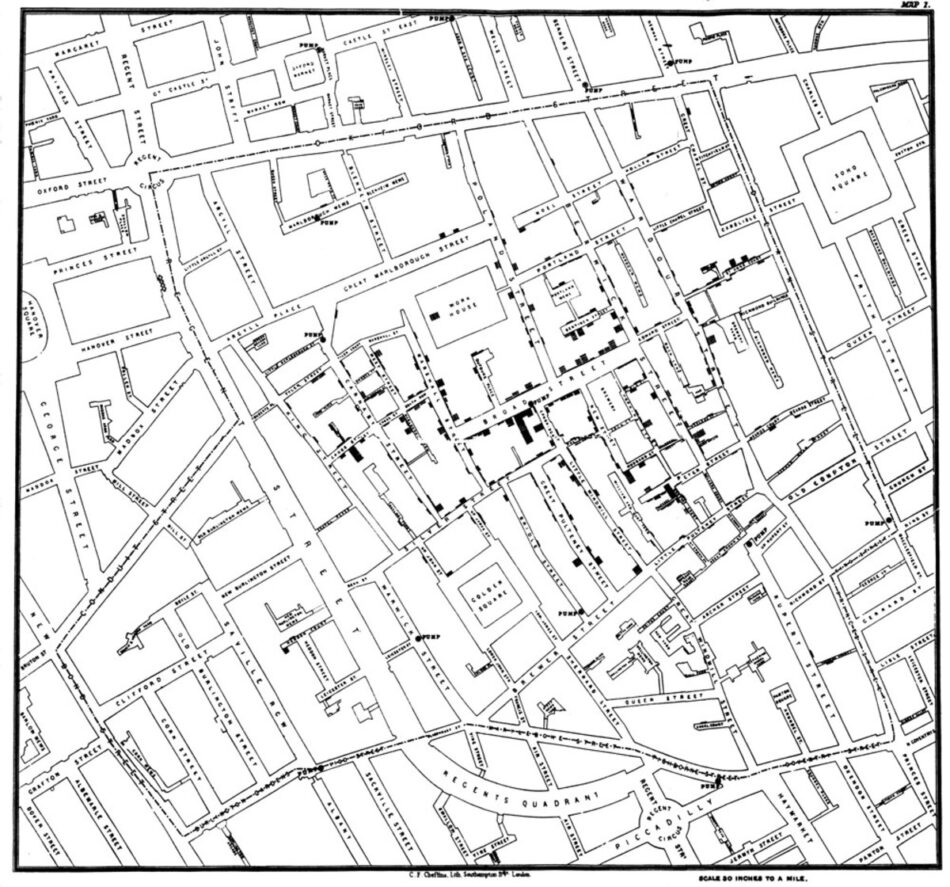
Snow’s approach to extrapolation was novel. Instead of emptying the city—as had been done in prior outbreaks—he took out a map of Soho and placed a dot where each cholera case had emerged. At the largest cluster of dots—a clear nucleus—Snow found a local water pump with a broken sewer pipe dumping human waste into that drinking water. When he had the handle of the pump removed, the outbreak in the area declined.
Cholera was not morally borne but waterborne. And those roads and alleyways, and the pipes laid beneath them and buildings built among them, were causing disease.
Snow’s simple mapping method became a foundational document for understanding disease and the design of our cities. He is cited as a founding father of epidemiology and urban design alike, showing proof that without proper urban planning, the public’s health is at grave risk. He also revealed a structural solution that was blind to class, linking the worker’s health to the health of the public at large. Such conclusions inspired a redesign of the piped city substructure, increased zoning and regulatory superstructure, and the decongestion of dense tenement housing in industrial capitals such as London and New York for the latter part of the 19th century. More conceptually, however, what Snow revealed was that our biological survival was spatially reliant.
The Sanitation Movement: Design Solutions Addressing Disease
Other designers took notice. In 1854, with the Crimean War raging, injured soldiers in hospital barracks were contracting diseases like dysentery, typhoid, malaria, and cholera. Isambard Kingdom Brunel—the engineer of the first underwater tunnel and other marvels of construction—dreamed up a new hospital design to help stem disease. His Renkioi Hospital arrived flat-packed and prefabricated on train beds. When constructed, the wards were lifted off the ground on small legs, which separated waste from inhabitants. The distances between enclosures as well as the height of rooms and their window orientation were calibrated to force air to flow and light to shine. And numerous hand sinks and toilets encouraged hygienic care. Brunel’s design suggested that a more proscriptive architecture could encourage sanitary behavior and thus improve health. And as the death rate dropped from 43 percent to a stunning 3 percent, his hypothesis was validated.3 Better buildings could change behavior and thus health. The converse must also be true: poorly designed places could injure.
Despite being a temporary structure, Renkioi Hospital’s principles had a permanent impact. Florence Nightingale, then a nurse mending wounds in the Crimean conflict, translated Brunel’s experiments into building guidelines in her 1859 book Notes on Hospitals. She prescribed tight configurations for air and light manipulations, immediately influencing newly constructed clinics and almshouses throughout London. Her work had an almost instant impact on overall public health. Rates of diseases like cholera and tuberculosis dropped and the design of new houses and hospitals soared. The so-called Nightingale ward shaped a new breed of hospital design that was cognizant of the contagious air and bodies within. The pavilion-plan hospital—which often included a dedicated Nightingale ward—would go on to become the dominant hospital typology for the next half century and inextricably link the design of buildings to the public’s health.
The Rise of the Modern City
The modern city did not emerge from the heroic feats of engineering and stricter municipal planning alone; there was also a fundamental shift in modern thinking. As Shapin argues, urban dwellers began to understand their lives as interrelated and codependent: “[People were] no longer subject to the caprices of divine will but a human environment whose well-being was in the care of human institutions and the expert knowledge contained within those institutions.”4 The modern city required larger-scale municipal departments to keep the polis healthy. And reform agendas spanned the globe to offer public infrastructure investment as a solution to the radical reduction of communicable diseases like cholera and tuberculosis. At the end of the 19th century, cholera rates were so low that disease outbreaks were found almost exclusively in the extremely rainy climates of Southeast Asia, where cholera constantly simmered as an endemic disease.5
However, this success turned out to be cholera’s nadir. Through the colonial era, foreign sponsorship of public infrastructure was a common form of technocratic control and resource safeguarding. But as colonies became independent, infrastructural investments from previous colonial powers and new multilaterals like the World Bank waned in favor of debt and neoliberal restructuring. As Mike Davis noted in his book Planet of Slums, “economic globalization without concomitant investment in a global public-health infrastructure is a certain formula for catastrophe.”6 And catastrophe struck. In the 1970s an outbreak of cholera surged across central Africa. In the 1990s, another epidemic canvassed Latin America. And by the turn of the 20th century, endemic cases were once again recorded in almost every country on earth.

Cholera in Haiti
When I flew to Haiti in 2011, the consequences of decades of political instability and economic insecurity were spatially visible. Sixty percent of the city’s three million people lived in slums. If people had toilets, they rarely con- nected to sewers. And whatever collection systems remained were either rogue or privatized—rendering access grossly inequitable. A large amount of the waste eventually found its way into drainage canals built by the US Army Corps of Engineers in the 1950s—a remnant of a previous era of American infrastructure investment into allied nation-states. These canals gather rainwater and any refuse the rainwater drags down from the mountainous backdrop of Port-au-Prince, cutting deep gouges through the city bowl and spilling countless detritus into the Caribbean Sea. One canal terminates under the large seaside promenade named Boulevard Harry Truman. Opened in 1949—the 200th anniversary of the founding of Port-au-Prince and the launch of Haiti’s international exposition—it was designed as an ocean wall and pedestrian promenade. Boulevard Harry Truman is a primary example of how foreign infrastructure investments were once common—but also how they were intended to be symbols of political alignment—a more tightly woven blanket with “From the American People” stamped all over it.
These were some of the last major infrastructure investments, and instead of an oceanfront promenade, today a delta has formed around the boulevard and an enormous landmass sits beyond it. That landmass is composed of 60 years of garbage, silt, and waste runoff from that canal. Cité de Dieu—or City of God, as the neighborhood is called—hosts over 50,000 residents on top of that mound with barely a waste or water pipe to connect to.
Without the corresponding investments needed to main- tain infrastructure like the boulevard, the canals, or new neighborhoods like Cité de Dieu, what has resulted is a place unprepared for its population growth and unable to afford its required sanitation infrastructure needed to support it. Poor planning, poor design, and poor investment have led to a city that is the most vulnerable in the face of epidemic or ecological disruption. And yet, here, among so much vulnerability, Cité de Dieu residents fared much better than other neighborhoods against cholera.
A modest hospital campus sits on Boulevard Harry Truman; it opened in response to another epidemic—HIV—in 1981, when Dr. Jean William Pape launched Les Centres GHESKIO, an everything-it-takes organization to cure the particular diseases emerging in Haiti. It was the world’s first HIV/AIDS clinic, and GHESKIO (which stands for, in French, Group for the Study of Kaposi’s Sarcoma Opportunistic Infections) has since opened the most advanced research lab in the Caribbean and a chlorine factory to decontaminate water, and initiated broad, community-based education programs aimed at eliminating the risks of open waste and dirty water. At the height of the cholera outbreak in 2010, Pape opened a temporary cholera treatment center in a tent and initiated a vaccine that international NGOs said was too expensive to administer. His teams nonetheless distributed chlorine caplets and water jugs to Cité de Dieu residents to ensure compliance and awareness. His rates of success were unprecedented, and not a single case of cholera has emerged from this neighborhood in almost a year. Meanwhile, outside his catchment area, he has treated nearly a quarter of the entire city’s cases. There were limits to his reach, however, most notably the modest campus and the spatial constraints of the tent facility that had stood far past its “temporary” expiration date. To expand his work, Pape needed a building.
Even though the outbreak has subsided and the citywide emergency tents have been taken down, Pape saw a need for permanent architecture that would prevent future outbreaks. At the time, my firm was already working with Pape on a tuberculosis hospital destroyed in the earthquake. When he approached us to help with the cholera center it occurred to us that the building needed to anticipate a flaring patient load but also address the glaring inadequacies of the sanitation system at large. Like the Nightingale wards of the 19th century that sought to address airborne disease, this center sought to address waterborne disease by collecting and decontaminating its own waste. This off-the-grid solution is not the solution to cholera, but it is an example of a structural patch that architecture can offer—an example, a prototype, a messenger to be replicated and learned from.
Pape taught us that a building is the interface of the system beneath it—a signpost for health, a beacon for structural change. A building must do more than house workers; it is never shelter from the storm if the storm brews from underneath. Instead, it must secure our peace of mind and it must be beautiful. This was part of his vision, as he later explained: “A building that is ugly, with no fresh air, no dignity or common sense, is a place people will avoid, and this encourages epidemics.”7 When people face death, their dignity is tested, “architecture and health are inseparable.”8
If Snow taught us the biological reason for cholera, and Brunel gave us engineering strategies to prevent it, Pape shows us is that in the modern city, behavior change and human dignity are core requirements for infrastructural change. He shows us that architecture is not a trade; instead it trades in the currency of dignity. Beauty can be a weapon against poverty, and we can begin to heal and solve the structural chasms that lie beneath our broken built environments when individual faces of these nameless masses are understood as mothers and sons and cousins.
Standing on Boulevard Harry Truman, hearing the quotidian calls of hawkers and tap-tap horns, watching the sunset before me, I thought of what Soho must have looked like when Snow canvassed that neighborhood in search of his water pump. “European cities, too, once looked like this,” Pape said to me. Places change constantly. And then it dawned on me that in GHESKIO, and in this doctor, was our creative fixer—a designer, a mapper, a maker—penning new structural solutions for the new urban metropolis. Behind me was the John Snow of our era, and the design solutions developed here could change how we consider the city, how we address our most intractable problems, and how we imagine a better world for those most vulnerable by using all of the disciplines at our disposal—including architecture.
2. Charles E. Rosenberg in ibid.
3. See John D. Thompson and Grace Goldin, The Hospital: A Social and Architectural History (New Haven, CT: Yale University Press, 1975), 205.
4. Shapin, “Sick City.”
5. See World Health Organization (WHO), “WHO Report on Global Surveillance of Epidemic-Prone Infectious Diseases,” http://www.who.int/csr/resources/publications/surveillance/en/cholera.pdf.
6. Mike Davis, Planet of Slums (London: Verso, 2006), 150.
7. Dr. Pape quoted in Michael Kimmelman, “In Haiti, Battling Disease with Open-Air Clinics,” New York Times, December 28, 2014, http://www.nytimes.com/2014/12/29/arts/design/in-haiti-battling-disease-with-open-air-clinics.html.
8. Ibid.
Michael Murphy is executive director of MASS Design Group. He holds a BA in English Literature and Language from the University of Chicago and an MArch from the Harvard University Graduate School of Design. He sits on the boards of the Clinton Global Initiative Advisory Committee and the Center for Health Care and Design.


